Hospital Version Of Health Reform Presentation Today
- 1. Health Care Reform: How Will it Change the Delivery System? SOUTH CAROLINA HOSPITAL ASSOCIATION 4/1/2010
- 3. Today’s Talk Historical Background Gaps in the US Healthcare System Goals of Health Care Reform How Reform Will Affect Consumers How Reform Will Affect Employers How Reform Will Affect Hospitals What’s Next?
- 4. Evolution of U.S. Health Care Policy Our system is the result of several major policy decisions rather than one, unified health care policy. Employer-based coverage Government-sponsored coverage EMTALA
- 5. Employer-Based Coverage During WWII, wage controls by the federal government led employers to offer health insurance instead of raising wages.
- 6. Medicare & Medicaid To cover the elderly and some of the very poor, the federal government enacted Medicare & Medicaid in mid 1960s.
- 7. EMTALA The Emergency Medical Treatment and Active Labor Act (EMTALA) of 1986 requires hospitals to screen and stabilize (treat) each and every patient who comes to the hospital ED seeking care.
- 8. Policy Decisions Have Left a Gap in Coverage for SC 2.2 million have employer-based health insurance 1.2 million rely on a government-sponsored program for coverage 178,000 have coverage purchased in the individual market 760,000 South Carolinians have no coverage *Source: Kaiser Family and Robert Wood Johnson Foundations
- 9. A Closer Look at South Carolina’s 760,000 Uninsured 557,000 live in working families that pay taxes to support government coverage for others 357,000 live at or below 133% of the federal poverty level SC has no program to help childless adults *Source: Kaiser Family Foundation
- 10. What Happens When the Uninsured Need Care? Remember EMTALA? Last year, SC hospitals provided more than $1 billion worth of care for which they received no direct payment. Those financial losses were passed along to insured patients and their employers.
- 11. Premiums Are Growing Faster Than Paychecks
- 12. Patient Protection and Affordable Care Act On March, 23, 2010, the Patient Protection and Affordable Care Act was signed into law.
- 14. “ Everyone is entitled to his own opinion, but not his own facts.” Senator Daniel Patrick Moynihan
- 16. The Myths You’ll have no choice in what health benefits you receive; a “health choices commissioner” will decide what benefits you get. Death panels will decide who lives. Illegal immigrants will get free health insurance. Federal funding of abortions will increase. Care will be rationed.
- 17. The Facts The new law will expand coverage to almost 500,000 of the 760,000 uninsured South Carolinians. No government-run, public option included. The new law includes health insurance reforms intended to protect consumers. The new law includes delivery system reforms that hold great promise for improving care.
- 18. 2010 Federal Poverty Levels 100% 133% 150% 200% 300% 400% Individual $10,830 $14,404 $16,245 $21,660 $32,490 $43,320 Family of 4 $22,050 $29,327 $33,075 $44,100 $66,150 $88,200
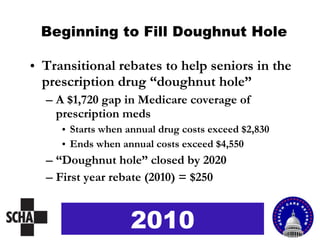
- 20. Provisions Going Into Effect in 2010 Temporary high risk pool for persons with pre-existing conditions and non-Medicare eligible retirees over 55 Transitional rebates to fill “doughnut hole” First round of insurance reforms 2010
- 21. High Risk Pool Temporary high risk pool to cover persons with pre-existing conditions and non-Medicare eligible retirees over 55 2010
- 22. Beginning to Fill Doughnut Hole Transitional rebates to help seniors in the prescription drug “doughnut hole” A $1,720 gap in Medicare coverage of prescription meds Starts when annual drug costs exceed $2,830 Ends when annual costs exceed $4,550 “ Doughnut hole” closed by 2020 First year rebate (2010) = $250 2010
- 23. First Round of Insurance Reforms No cancellation of coverage when an insured person becomes sick No denial of coverage for children with pre-existing conditions Young adults up to age 26 may remain on parents’ policies No lifetime limits on coverage 2010
- 24. Provisions Going into Effect in 2014 Premium assistance and subsidies for consumers Health insurance exchanges Essential health benefits Medicaid expansion Additional insurance reforms Individual mandate 2014
- 25. Premium Assistance For low income persons with incomes between 133 – 400% of federal poverty level 2014 If you make: You will pay: Assuming avg premium for family of 4 = $13,000 100-150% FPL 6% of premiums or $780 150-200% FPL 15% of premiums or $1,950 200-250% FPL 27% of premiums or $3,510 250-400% FPL 30% of premiums or $3,900
- 26. Out-of-Pocket Limits The law will limit the amount any person buying through the Exchange will have to pay out-of-pocket. Limits will be tied to federal government’s HSA limits, as follows: 2014 If you make: You won’t pay more than: Based on 2010 HSA limits 100-200% FPL ⅓ HSA limits $1,983 ind/$3,967 family 200-300% FPL ½ HSA limits $2,975 ind/$5,950 family 300-400% FPL ⅔ HSA limits $3,987 ind/$7,973 family
- 27. To make it easier to shop for affordable policies To offer essential benefits as defined by HHS To serve businesses with fewer than 100 workers, self-employed, and unemployed To include a multi-state insurance plan similar to federal employee benefit plan To offer coverage to larger businesses beginning 2017 Health Insurance Exchanges 2014
- 28. Health Insurance Exchange Links buyers and sellers of insurance Insurance “Exchange” or “Connector” Uninsured (Not eligible for Medicaid/CHIP) Self Employed Small Business Others Private Plan Private Plan Private Plan Private Plan
- 29. Essential Health Benefits Effective 1/1/2014, creates package that includes comprehensive set of services Must cover at least 60% of actuarial value of covered benefits Limits annual cost sharing to current HSA limits Requires all qualified health benefit plans to offer at least the essential package 2014
- 30. Medicaid Expansion By 2014, states must extend Medicaid eligibility to all legal residents up to 133% of poverty and under 65 years old. 133% FPL is $14,404 for individual and $29,327 for family of 4. Feds will cover 100% of states’ costs from 2014-2016 and the following portions after 2016: 2017 – 95% 2018 – 94% 2019 – 93% Beyond – 90% 2014
- 31. Additional Insurance Reforms No annual limits on coverage No denial of coverage for adults with pre-existing conditions No higher premium based on gender or medical history Insurers required to report share of premium income spent on medical care Limits on out-of-pocket costs 2014
- 32. Individual Mandate Beginning Jan. 1, 2014, US citizens and legal immigrants must have coverage or pay a penalty when they file their federal tax returns. Individual penalties $95 per person in 2014 $325 per person in 2015 $695 per person in 2016 Household penalties 1% of household income in 2014 2% of household income in 2015 2.5% of household income in 2016 *Exemptions for hardship 2014
- 33. Insurance Reforms & the Individual Mandate Many of the popular insurance reforms work only if we have an individual mandate. Why? If you could buy auto insurance the day you had an accident, would you buy it beforehand? If you could buy homeowners insurance the day your house burned down, would you buy it beforehand? If you could buy health insurance the day you were diagnosed with cancer, would you buy it beforehand? If only sick people bought insurance, what would happen to the premiums?
- 35. Provisions Affecting Employers Provides tax credits to small businesses that purchase health insurance for employees (2010) Allows young adults up to 26 to remain on parents policies (2010) Requires employers to report health care benefits value on W-2 forms (2011) Pay or play for large employers (more than 50 workers) (2014) Allows large employers to provide coverage through state exchanges (2017) Imposes 40% excise tax on Cadillac plans (2018)
- 36. Tax Credits for Small Employers Tax credits for small employers with less than 26 workers paying at least half of their workers’ health premiums Phase I provides tax credit up to 35% of employer’s contribution (tax years 2010 – 2013) Phase II provides tax credit up to 50% of employer’s contribution (tax years 2014 and beyond) Amount of tax credit varies with firm size and average wage 2010
- 37. Pay or Play for Large Employers Large employers (more than 50 workers) not offering coverage will pay $2,000 per year per worker minus first 30 full-time employees. Employers with 50 or fewer employees are exempt. 2014
- 39. Provisions Affecting Hospitals Payment Access Quality Other
- 40. Medicare & Medicaid Payment Cuts Nationally, hospital payments will be cut $155 billion over 10 year period beginning in 2010 to help pay for expanding coverage to 32 million. Medicare update factors to hospitals will be reduced by $112 billion beginning 2010 Medicare DSH will be reduced $22 billion beginning 2014 Medicaid DSH will be reduced $14 billion beginning in 2014
- 41. Other Payment Changes (in order they take effect) Expands 340B drug discount to outpatients at children’s, cancer and critical access hospitals, as well as sole community hospitals and rural referral centers (2010) Prohibits federal payments to states for Medicaid services related to health care acquired conditions (2011) Allocates $400 million for additional payments to hospitals in counties with lowest Medicare spending (2011 and 2012)
- 42. Other Payment Changes . . . continued Requires plan for reforming hospital wage index system (2012) Reduces Medicare payment for excess readmissions (2013) Establishes budget-neutral Medicare Value-Based Purchasing Program (2013)
- 43. Other Payment Changes . . . continued Establishes Independent Payment Advisory Board (IPAB) to submit proposals to reduce Medicare spending (2014) Most hospitals exempt for first 10 years Requires penalties and public reporting on health care acquired conditions for Medicare patients (2015)
- 44. Improving Access to Primary Care (in order they take effect) Establishes Teaching Health Centers to provide Medicare payments for primary care residency programs in federally qualified health centers (2010) Adds $11 billion for community health centers and the National Health Service Corps over five years (2011) Establishes new programs to support school-based health centers and nurse-managed health clinics (2011)
- 45. Improving Access to Primary Care . . . continued Provides 10% Medicare bonus payment to primary care physicians and general surgeons practicing in shortage areas (2011-2015) Increases Medicaid payments to primary care physicians to 100% of Medicare payment rates for two years (2013-2014) Increases graduate medical education slots for primary care by redistributing unused slots
- 46. Improving Access in Rural Areas Extends outpatient hold-harmless payments for certain hospitals in rural areas Improves payments for low-volume hospitals Ensures that CAHs are paid 101 % of costs for all outpatient services
- 47. Improving Access in Rural Areas . . . continued Extends and expands the Rural Community Hospital Demonstration Program Extends the Medicare Dependent Hospital program for one year Extends the Medicare Rural Hospital Flexibility Program through 2012 Extends reasonable cost reimbursement for laboratory services in small rural hospitals
- 48. Improving Quality (in order they take effect) Supports comparative effectiveness research (2010) Improves care coordination for dual eligibles (2010) Establishes Center for Medicare and Medicaid Innovation within CMS to improve coordination, quality, and efficiency (2011)
- 49. Improving Quality . . . continued Creates new Medicaid medical home option for enrollees with chronic conditions (2011) Establishes voluntary, national pilot program allowing groups of providers to be recognized as Accountable Care Organizations (ACOs) (2012)
- 50. Improving Quality . . . continued Requires enhanced data collection, reporting, and analysis to identify and monitor trends in health disparities (2012) Establishes national pilot program for Medicare payment bundling (2013)
- 51. Medicaid Payment Demonstrations Authorizes new Medicaid payment demonstrations (2010-2016) To make global capitated payments to safety net hospital systems (effective FY 2010-2012) To pay bundled payments for episodes of care that include hospitalizations (effective CY 2012-2016
- 52. Medicaid Payment Demonstrations… continued To allow pediatric medical providers to share in cost-savings (effective CY 2012-2016) To provide Medicaid payments to free-standing psych hospitals (IMD exclusion) for adult enrollees who require stabilization of an emergency condition (effective 10/1/2011 thru 12/31/2015)
- 53. Other Provisions Impacting Hospitals Establishes Workforce Advisory Committee to develop national workforce strategy (2010) Increases workforce supply and supports training of health professionals through scholarships and loans (2010)
- 54. New Requirements for Maintaining 501(c)(3) Status Effective for taxable year 2011, hospital must: Implement strategies to meet community needs based on health needs assessment Develop, implement, communicate a charity care policy Limit charges to those qualifying for financial assistance To lowest amounts charged to individuals with insurance Restricts use of extraordinary collection actions $50,000 penalty to those who fail to comply!
- 55. Other Provisions Impacting Hospitals . . . continued Bans new physician-owned hospitals in Medicare (2010) Extends long term care hospital provisions in the Medicare, Medicaid and SCHIP Extension Act of 2008 Increases funding to fight fraud and abuse
- 56. Other Provisions Impacting Hospitals . . . continued Provides $50 million to states for medical liability reform demonstrations (2011) Simplifies health insurance administration (2013-2014)
- 57. What Happens Now? The new law contains broad concepts and requirements, but the details will come with regulations . Regulations will be drafted by a variety of federal agencies, and interested persons will need to track the proposed regulations carefully. In short, there’s still a lot of work to be done!
- 58. ANY QUESTIONS?
- 59. SOUTH CAROLINA HOSPITAL ASSOCIATION Health Care Reform For more information: www.scha.org/advocacy/health-care-reform 4/1/2010
Editor's Notes
- #3: Before we even begin , it’s important to remember that health care reform is VERY political.
- #6: Prior to World War II, health care didn’t cost much because we didn’t have much in the way of technology or medications. During the War, America imposed wage controls to prevent runaway inflation. There was a shortage of workers, and employers were encouraged to compete for workers by offering benefits such as health insurance, which was inexpensive. After the war, as the devastated European nations were rebuilding their infrastructure, they had little choice but to build health care systems through their governments. America, meanwhile, maintained its employer-based system.
- #7: In the 1960s, Congress realized that there were limitations to an employer-based health insurance model because some people don’t work. The result was the enactment of Medicare (federally funded) to cover the elderly and Medicaid (joint federal and state funding) to help cover the poor. America still had a draft in the 1960s, so most American men were required to serve in the military and were entitled to VA health benefits for life. So Medicaid was designed to cover women and children. Now that we’ve had a volunteer army for years, millions of adult men find themselves without insurance coverage even if they have full-time jobs because they are not eligible for VA benefits. Breakdown of current national payor mix: 52% Employer 28% Government 5% Individual 15% Uninsured
- #8: In 1986, Congress decided to address the problem of the uninsured by requiring that hospitals treat every person who walks into the emergency room, even if the person can pay nothing. This requirement covers all persons in America, even if they are here illegally. No other organization or individual – not even physicians – are required to treat anyone who comes into their building seeking care. Only hospitals. The EMTALA obligation on hospitals is unlimited, so hospitals cannot manage the budget impact by limiting the number of uninsured patients they will treat. It is also an unfunded mandate – an obligation imposed by government without providing any new dollars to cover the cost. As the cost of health care increases, the unfunded mandate on hospitals increases. It’s fair to say that EMTALA is one of the largest – if not the largest – unfunded mandate ever imposed by Congress on private business. Ironically, it was enacted through the now-controversial legislative process called budget reconciliation by a Democratic House and a Republican Senate and signed into law by President Reagan. So President Reagan in essence signed the law that guarantees every person living in America, legally or illegally, the right to health care. And President George W. Bush reinforced that policy when he said, “People have access to health care in America. After all, you just go to an emergency room.”
- #11: This may be a good place to highlight your community benefit numbers.
- #12: Hospitals do have to cover all of our costs, and our revenue source is the insured patient. So as hospitals provide care for which we are not reimbursed, we pass that along to our paying patients and their employers. This pushes insurance premiums higher and puts existing insurance coverage at risk as employers have to make tough decisions about dropping or decreasing coverage, or even reducing their workforce.
- #13: That brings us to the newly enacted Patient Protection and Affordable Care Act, which attempts to find a more rational and compassionate way to deliver and pay for care for America’s working poor.
- #14: It has a strong resemblance to the Massachusetts model.
- #15: The enactment of the health care reform law has been met by open hostility from those whose political views differ from supporters of reform. Hospital leaders have also been challenged for our support of reform. But it’s important to separate opinion from facts. Each of us is entitled to our own opinion but not our own set of facts. And unfortunately, there is a lot of misinformation being blasted at us every day. Hospitals did not support health care reform as a result of our political views. The hospital industry supported reform because hospitals have a legal obligation to care for patients that is unlike the obligation owed by any other business or individual. We are obligated to care for everyone, regardless of their ability to pay. We don’t have the luxury of basing our positions on what we believe the law should be. We know what the law is and what is required of our facilities. And as the number of uninsured continues to grow, we realize that state and federal governments are going to demand more of us than we can give. Given hospitals’ legal obligation under EMTALA, it should come as no surprise to anyone that hospitals have an opinion on federal legislation that will provide coverage to 32 million more Americans. We are not picking a political side in this debate. We are acting to preserve the health care delivery system so we can continue to fulfill our missions in our communities.
- #16: The public has been told a lot of scary things about health care reform.
- #17: One myth is that you’ll have no choice in what health benefits you receive—a “health choices commissioner” will decide what benefits you get. The legislation does create an essential health benefits package that provides a comprehensive set of services, covers at least 60% of actuarial value, and limits annual cost sharing. Effective Jan 1, 2014, all qualified health benefit plans, including those offered through the Exchanges and those offered in individual and small group markets outside the Exchanges, will have to include at least the essential health benefits package. Requirements will be floors, not ceilings—feds will have no say in how generous private insurance can be. Another popular myth designed to scare people is that death panels will decide who lives. In truth, the legislation expands Medicare coverage to include optional counseling on end-of-life care for any senior who requests it. Another myth is that Illegal immigrants will get free health insurance. The reality is that access to coverage through state-based exchanges is restricted to U.S. citizens and legal immigrants who are not incarcerated. Federal funding of abortions will increase, the critics say. The legislation prohibits abortion coverage from being required as part of essential health benefits package. It also requires insurers participating in Exchanges who wish to offer coverage for abortions to calculate and collect separate premiums for that coverage. Finally, we have all heard that care will be rationed under health-care reform. Under the current system neither public programs nor private insurance plans cover everything. And that will not change. The essential benefit package will help limit what can be deemed uncovered and the legislation does establish a non-profit institute to conduct, with assistance by expert advisory panels, research that compares clinical effectiveness of medical treatments. As a result, health care consumers will be able to get comparative information about health care treatments just like they currently get from Consumer Reports when they buy a television or a car.
- #19: These are the 2010 Federal Poverty Levels. You might want to jot a couple of these down as we’ll reference them frequently throughout the presentation. 100% of FPL for an individual is $10,830 per year 100% of FPL for a family of 4 is $22,050 per year
- #22: While many of the provisions will be phased in over the next several years, there are several provisions that will offer help in 2010. Theses include a temporary, federally funded high risk pool so people who cannot get insurance because they have a pre-existing condition will have an affordable option. The fund will expire in 2014 when pre-existing conditions are outlawed as a reason insurers can refuse to cover someone. Beginning this year, children can no longer be denied coverage for a preexisting condition. There is some consideration that existing state high risk pools (ie. SC) may serve as the foundation for this new temporary national pool.
- #23: We have heard a lot about the doughnut hole that many seniors on Part D Medicare face each year. They get Medicare assistance with their prescription drug costs until their total drug costs hit $2830. Then the seniors have to pay the next $1720 out of pocket. When their total climbs past $4550, Medicare will begin to help again. The $1720 that seniors have to pay out of pocket is known as the doughnut hole. Obviously, it places a tremendous burden on seniors living on fixed incomes and is often the reason some seniors decide not to take all of their their medications. A small step – a transitional rebate of $250 – will go into effect this year to help seniors once they reach the “doughnut hole”. With the phase in of other transitional steps over the next decade, the doughnut hole will be closed by 2020.
- #24: The law calls for significant insurance reform and the first steps begin this year as insurers are prohibited from cancelling coverage when someone becomes sick. I had mentioned earlier that insurers can no longer deny coverage to children with pre-existing conditions. And young adults up to age 26 will be able to remain on their parents’ health insurance policy. Also, beginning in 2010, health insurers can no longer impose a lifetime limit on coverage, which is great news for people with very serious illnesses and injuries. Note: No denial of coverage for adults with pre-existing conditions goes into effect in 2014 No annual limits on coverage goes into effect in 2014.
- #28: The multi-state health insurance plan (similar to Federal Employee Health Benefit Plan) will be administered by the federal Office of Personnel Management. The law also calls for the creation of Consumer Operated and Oriented Plan (CO-OP) program to foster the creation of non-profit, member-run health insurance companies in all 50 states and the District of Columbia to offer qualified health plans. (Appropriate $6 billion to finance the program and award loans and grants to establish CO-OPs by July 1, 2013)
- #30: Current HSA limits ($5,950 for individual and $11,900 for family)
- #31: This law removes all catogorical requirements changing Medicaid to an income based eligibility program.
- #37: This year, small employers will be eligible to claim tax credits depending on the number of employees and average wages, as long as the employer pays at least 50% of the employee’s premium. Additional notes regarding small business tax credits: – Phase I: For tax years 2010 through 2013, provide a tax credit of up to 35% of the employer’s contribution toward the employee’s health insurance premium if the employer contributes at least 50% of the total premium cost or 50% of a benchmark premium. The full credit will be available to employers with 10 or fewer employees and average annual wages of less than $25,000. The credit phases-out as firm size and average wage increases. Tax-exempt small businesses meeting these requirements are eligible for tax credits of up to 25% of the employer’s contribution toward the employee’s health insurance premium. – Phase II: For tax years 2014 and later, for eligible small businesses that purchase coverage through the state Exchange, provide a tax credit of up to 50% of the employer’s contribution toward the employee’s health insurance premium if the employer contributes at least 50% of the total premium cost. The credit will be available for two years. The full credit will be available to employers with 10 or fewer employees and average annual wages of less than $25,000. The credit phases-out as firm size and average wage increases. Tax-exempt small businesses meeting these requirements are eligible for tax credits of up to 35% of the employer’s contribution toward the employee’s health insurance premium.
- #38: Assesses a fee if employer has at least one FTE receiving a premium tax credit Imposes penalties on employers providing “unaffordable” coverage Requires employers with more than 200 employees to automatically employees into health insurance plans offered by employer. Employees may opt out
- #41: In return for expanded coverage for 32 million uninsured, The American Hospital Association, Catholic Hospital Association, Federation of American Hospitals agreed to $155 billion in reduced spending for Medicare and Medicaid hospital services over 10 years. Medicare update factors For 2010 (beginning April 1) and 2011, the Medicare hospital payment update would be reduced by 0.25% Beginning in 2012, the market basket would be reduced by an estimate of productivity, with added reductions of 0.1% in 2012 and 2013, 0.3% in 2014, 0.2% in 2015 and 2016, and 0.75 % in 2017, 2018 and 2019 In 2020 and beyond, hospital payment updates would be reduced by productivity. The deeper reductions would apply to inpatient hospital, outpatient hospital, inpatient rehabilitation, inpatient psychiatric, and long-term care hospitals. The update reductions would not sunset and would not be protected from going below zero. Medicare DSH Reduces Medicare DSH payments by 75% to eliminate DSH payments that are above the “empirically justified” level, as determined by the Medicare Payment Advisory Commission A portion of the 75% would then be returned to hospitals depending on the amount of uncompensated care they provide. This amount is subject to a trigger, and would be phased down if coverage increases. Medicaid DSH Medicaid DSH reductions are not directly tied to increases in the level of insurance coverage, and the final bill directs the Secretary to develop a methodology for reducing federal DSH allotments to all states in order to achieve the mandated reductions In making DSH reductions, the Secretary is instructed to look at a state’s percentage of reduction in the uninsured, and whether a state targets DSH funds to hospitals with high Medicaid volumes or uncompensated care.
- #42: 340 Drug Discount Program Extends eligibility for the 340B drug discount outpatient program to children’s, cancer and critical access hospitals, as well as certain sole community hospitals and rural referral centers. It does not expand the program for existing 340B hospitals to cover inpatient drugs It exempts orphan drugs from required discounts for new 340B entities. Geographic variation The new law allocates $400 million for payments for FYs 2011 and 2012 to section 1886(d) hospitals located in counties that rank in the lowest quartile for age, sex and race adjusted per enrollee spending for Medicare Parts A and B. The payments would be proportional to each hospital’s share of the sum of Medicare inpatient PPS payments for all qualifying hospitals. Includes a commitment by the Secretary to commission two Institute of Medicine studies and convene a National
- #43: Wage index The hospital wage plan would be required to take into account the 2001 MedPAC wage index report, including the proposed use of Bureau of Labor Statistics data and the recommended redefinition of wage areas. Would establish, with new funding, a hospital wage index floor of 1.0 for inpatient and outpatient services and a practice expense floor of 1.0 for physicians in “frontier” states (Montana, Nevada, North Dakota, South Dakota and Wyoming) Readmissions Medicare will impose financial penalties on hospitals for so-called “excess” readmissions when compared to “expected” levels of readmissions based on the 30-day readmission measures for heart attack, heart failure and pneumonia that are currently part of the Medicare pay-for reporting program. Excludes critical access hospitals and post-acute care providers. Establishes assistance program for hospitals with high readmissions. Performance Level Comparisons (Weighted Averages for 30-day readmissions) All US Hospitals South Carolina 19.2% Heart Attack 18.6% 24.4% Heart Failure 23.9% 18.3% Pneumonia 18.0% DATA SOURCE: Haneys: Medicare Data that reflects aggregate data for three years: July 1, 2005 through June 30, 2008. Value-based Purchasing The Value Based purchasing program is budget neutral, with 1 percent of payments allocated to the program in FY 2013, growing over time to 2 percent in 2017 and beyond. Efficiency measures to be added (approach to address geographic variation in spending). Prohibits use of readmissions measures. Would establish demonstration project to test value-based purchasing (VBP) model for CAHs.
- #44: IPAB PPS Hospitals (but not Critical Access Hospitals) are exempt from IPAB’s recommendations for ten years. Targeted amounts are 0.5 percentage point reduction in 2015, increasing to a 1.5 percentage point reduction in 2018. Congress could modify or pass an alternative to the proposals, but would be required to maintain the targeted level of Medicare savings for the year. IPAB’s original proposal would be implemented if Congress does not consider the board’s proposal. IPAB to make non-binding recommendations on system-wide costs. HAC Hospitals in the worst 25th percentile of risk-adjusted HAC rates would be subject to a 1.0% payment penalty under Medicare. The reduction would be applied in addition to current CMS payment adjustments for HACs. The Secretary would be required to study and report to Congress by January 1, 2012, on expanding the HAC policy to inpatient rehabilitation facilities, long-term care hospitals, hospital outpatient departments, and other hospitals excluded from the Inpatient PPS.
- #46: Medicare bonus payment to primary care phsysicians and general surgeons The bonus payments will be directed to primary care physicians and general surgeons practicing in Health Professional Shortage Areas (HPSAs) designated by HHS. Medicaid payments to primary care physicians Requires that Medicaid payment rates to primary care physicians for furnishing primary care services be no less than 100% of Medicare payment rates in 2013 and 2014 (the first year of the Senate bill’s Medicaid coverage expansion to all individuals with incomes under 133% of FPL). Provides 100% federal funding to states for the incremental costs of meeting this requirement. Graduate Medical Education Redistributes 65% of the currently unused GME training slots. Rural hospitals with less than 250 beds and hospitals that participated in voluntary reduction programs are exempt from reductions. Hospitals could apply to receive up to 75 additional residency positions. In return, the hospital would be required to use at least 75% of the increase for primary care or general surgery residency and to maintain its quantity of primary care residents. Program enhancements for counting residency time in non-hospital settings. No cuts to GME payments to hospitals.
- #47: Notes
- #49: Comparative Effectiveness Research Establishes non-profit Patient-Centered Outcomes Research Institute to compare clinical effectiveness of medical treatments Institute to be overseen by multi-stakeholder Board and assisted by expert advisory panels Dual eligibles Creates new Federal Coordinated Health Care Office within CMS to integrate Medicare and Medicaid benefits Goal to improve access to and quality of care and services for dual eligibles Innovation Center Center will test innovative payment and service delivery models. After testing, the HHS Secretary could expand the scope and duration of a model. Allows the Secretary to test innovative payment and service delivery models within certain geographic areas.
- #50: Medical home Enrollee must have two chronic conditions, one condition and risk of developing another, or at least one serious and persistent mental health condition. Provides states taking up the option with 90% FMAP for two years. ACOs ACOs would be responsible for managing the care of certain beneficiaries. Hospitals could take the lead in formation an ACO. Hospitals and other providers of the ACO could share in Medicare cost savings they achieve. The Secretary would reset spending benchmarks after three years.
- #51: Health Disparities Requires enhanced collection and reporting of data on race, ethnicity, sex, primary language, disability status, and for underserved rural and frontier populations Requires Secretary to analyze data to monitor trends in disparities Medicare Bundling Pilot program to develop and evaluate paying bundled payment for acute I/P hospital, physician, O/P hospital, and post-acute care services for episode of care that begins 3 days prior to hospitalization and spans 30 days following discharge If pilot achieves goals of improving or not reducing quality and reducing spending, develop plan for expanding pilot program by 1/1/2016
- #53: IMD pilot project Includes a $75 million grant proposal to establish a three-year demonstration program for approved states to allow coverage for Medicaid patients in freestanding psychiatric hospitals.
- #54: Notes
- #56: Physician-owned hospitals Requires compliance with disclosure, patient safety, bona fide investment, and growth restriction rules. Provides limited exceptions to the growth restrictions for grandfathered physician-owned hospitals including a new exception for hospitals that treat the highest percentage of Medicaid patients in their county (and are not the sole hospital in a county). Long Term Care Extends specific provisions for two years. Would further delay full implementation of the 25% Rule, the short-stay outlier cuts, and the one-time budget-neutrality adjustments planned by CMS. Extends current moratorium on new LTCH beds and facilities, with exceptions. Fraud and Abuse Establishes new requirements and penalties for providers, suppliers and others Increases financial penalties for submitting false claims Develops data base to capture and share data across federal and state programs
- #57: Medical Liability Reform Authorizes the Secretary to award five year demonstration grants to states to develop, implement, and evaluate alternatives to existing tort litigation system. Preference to be given to states that: have developed alternatives in consultation with relevant stakeholders have proposals that are likely to enhance patient safety by reducing medical errors and adverse events are likely to improve access to liability insurance Administrative simplification Expands administrative simplification provisions under HIPAA by HHS for greater uniformity and reduction of administrative costs Requires health plans to comply with single set of operating rules for eligibility verification, claims status. Electronic funds transfers, health care payment and remittance, health encounter information, enrollment/disenrollment, premium payments, and referral certification and authorization