Neutropenic fever : Challenges and Treatment
- 1. Neutropenic Fever: Challenges and Treatment Dong-Gun Lee Div. of Infectious Diseases, Dept. of Internal Medicine, The Catholic Univ. of Korea
- 2. Contents • Epidemiology Focus in Asia ; Etiologic microorganisms & Resistance • ESBL producing Enterobacteriaceae • Glycopeptides
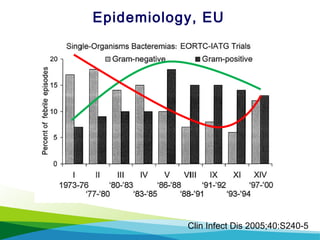
- 3. Clin Infect Dis 2005;40:S240-5 Epidemiology, EU
- 4. Clin Infect Dis 2003;36:1103-10 Epidemiology, US [SCOPE] Project
- 5. Epidemiology, Malaysia (2004) Int J Infect Dis 2007;11:513-7
- 7. Epidemiology, Taiwan (‘02-06) Epidemiol Infect 2010;138:1044;51
- 8. Korean J Intern Med 2011;26:220-52 Infect Chemother 2011;43:285-321 NA09-013
- 9. 초기 항균요법 (2) No. (%) Reference Rho et al. Rhee et al. Choi et al. Kim et al. Park et al. Period (year) 1996-2001 1996-2003 1998-1999 1999-2000 2001-2002 Hospital A B C D C Patients leukemia allo-HSCT acute leukemia cancer HSCT Prophylaxis NA Cotrimazole Nystatin gargle Ciprofloxacin, roxithromycin, fluconazole NA Ciprofloxacin, fluconazole/ itraconazole, TMP/SMX No. of MDI 27 (100) 78 (100) 158 (100) 42 (100) 72 (100) Gram (+) bacteria 11 (40.7) 36 (46.2) 75 (47.5) 11 (26.2) 25 (34.7) Streptococcus 1 (3.7) - 24 (15.2) 2 (4.8) 9 (12.5) CoNS 4 (14.8) 15 (19.2) 20 (12.7) 4 (9.5) 7 (9.7) Staphylococcus aureus 4 (14.8) - 13 (8.2) 3 (7.1) 2 (2.8) Enterococcus 2 (7.4) - 14 (8.9) 2 (4.8) 6 (8.3) Gram (-) bacteria 16 (59.3) 42 (53.8) 83 (52.5) 31 (73.8) 47 (65.3) Escherichia coli 4 (14.8) - 43 (27.2) 2 (4.8) 32 (44.4) Pseudomonas aeruginosa 1 (3.7) - 12 (7.6) 5 (11.9) 4 (5.6) Klebsiella pneumoniae 6 (22.2) - 12 (7.6) 8 (19.0) 4 (5.6) Enterobacter - - 5 (3.2) 4 (9.5) 3 (4.2) Acinetobacter baumanii 2 (7.4) - - 2 (4.8) 2 (2.8) Aeromonas hydrophila 1 (3.7) - 6 (3.8) - - Citrobacter freundii - - - 2 (4.8) 1 (1.4) Salmonella - - - 4 (9.5) - Epidemiology, Korea
- 10. Catholic HSCT Center (Pre-engraftment) ’83 ~ ’88 ’89 ~ ’92 ’93 ~ ’96 ’98 ~ ’99 ’01 ~ ’02 No. of isolates 13 14 8 24 25 G (+) CNS (6) CNS (6) S. aureus (4) S. epidermidis (10) Streptococcus (9) S. aureus (2) S. aureus (3) S. epidermidis (3) Streptococcus (5) CNS (7) Enterococcus (3) Enterococcus (2) E. faecalis (1) Staphylococcus (3) S.aureus (2) Streptococcus (2) Streptococcus (3) E. faecium (4) E. faccium (4) E. faecalis (2) E. faecalis (2) Micrococcus (1) 15 12 24 40 47 G (-) P. aeruginosa (11) P. aeruginosa (8) P. aeruginosa (6) E. coli (32) E. coli (32) Klebsiella (2) Klebsiella (1) E. coli (5) Klebsiella (3) K. pneumoniae (4) E. coli (1) E. coli (1) Enterobacter (5) Enterobacter (2) P. aeruginosa (4) Other (1) Others (2) Klebsiella (3) P. aeruginosa (1) Enterobacter (3) Others (5) Others (2) A. baumanii (2) Epidemiology, Catholic BMT Center (Pre-engraftment Period) J Korean Med Sci 2006;21:199-207
- 11. ’83 ~ ’ 88 ’89 ~ ’ 92 ’93 ~ ’ 96 ’98 ~ ’ 99 ’01 ~ ’ 02 Others Enterobacter spp. K. pneumoniae E. coli P. aeruginosa 0 10 20 30 40 50 60 70 80 GNB Catholic HSCT Center (Pre-engraftment) Epidemiology, Catholic BMT Center
- 12. Catholic HSCT Center (Pre-engraftment) ’83 ~ ’88 ’89 ~ ’92 ’93 ~ ’96 ’98 ~ ’99 ’01 ~ ’02 Enterococcus spp. Streptococcus spp. S. aureus CNS 0 10 20 30 40 50 GPC Epidemiology, Catholic BMT Center
- 13. Organisms (n=243) Ward A Ward B Total (%) P value Gram (+) (n=122) (n=108) (n=14) S. aureus 9 2 11 (4.5) 0.649 CoNS 14 0 14 (5.8) 0.227 Viridians streptococci 39 (18.6) 5 (15.2) 44 (18.1) 0.635 S. pneumonia 2 0 2 (0.8) Rothia mucilaginosa 5 0 5 (2.1) Enterococcus spp. 27 7 34 (14.0) 0.198 Corynebacterium spp. 4 0 4 (1.6) Bacillus spp. 3 0 3 (1.2) Others† 5 0 5 (2.1) Gram (-) (n=119) (n=100) (n=17) E. coli 58 (27.6) 14 (42.4) 72 (29.6) 0.083 K. pneumonia 28 (13.3) 3 (9.1) 31 (12.8) Pseudomonas spp. 5 1 6 (2.5) Enterobacter spp. 3 1 4 (1.6) Stenotrophomonas maltophilia 4 0 4 (1.6) Others* 2 0 2 (0.8) Fungus (n=2) Candida tropicalis 1 0 1 (0.4) No. of microorganims Epidemiology, Catholic BMT Center (‘09-’10)
- 14. Pathogens (No. of isolates) No. of isolates resistant to antibiotics/no. of isolates tested PCV OXAC CLM EM CFTX CFPM GM CPFX or LVX VAN IMPM AMP S. aureus (11) 11/11 7/11 5/11 5/11 - - 4/11 6/11 0/11 - - CoNS (14) 14/14 12/1 3 8/14 9/14 - - 10/14 13/14 0/14 - - Streptococci other than pneumococcus (46) 24/46 - 11/45 21/46 4/45 17/45 - 0/1 0/45 - 0/2 S. pneumonia (2) 0/2 - - 2/2 0/2 - - 0/2 0/2 - - Enterococcus faecium (19) 19/19 - 19/19 17/19 - - - 19/19 7/19 19/19 19/19 Enterococcus faecalis (15) 6/15 - 15/15 12/15 - - - 14/15 0/15 0/15 5/15 Gamella mibiliform (1) 1/1 - 0/1 0/1 0/1 0/1 - - 0/1 - - Total no. of G (+) 75/10 8 19/24 58/105 66/108 4/48 17/46 14/25 52/62 7/107 19/34 24/36 % of resistance 69.4 79.2 55.2 61.1 8.3 37.0 56.0 83.9 6.5 55.9 66.7 Resistance Patterns (GPC) Resistance Pattern, GPC
- 15. Pathogens (No. of isolates) No. of isolates resistant to antibiotics/no. of isolates tested ESBL AMC PIPC GM TOB CAZ LVX SXT AZTN IMPM MRPN E. coli (72) 22/63 64/72 64/72 30/72 33/72 24/72 65/70 40/72 23/72 0/72 0/72 K. pneumoniae (31) 22/31 31/31 27/31 18/31 21/31 22/31 24/29 20/31 22/31 0/31 0/31 Pseudomonas spp. (6) - - 0/6 0/6 0/5 2/6 3/5 4/4 2/6 4/6 0/6 Enterobacter spp. (4) - 4/4 4/4 0/4 0/4 1/4 1/4 3/4 1/4 0/4 0/4 S. maltophilia (4) - - - - - - 0/4 0/4 - - - B. cepacia (1) - - - - - 0/1 0/1 0/1 - - 0/1 C. indologenes (1) - - 1/1 1/1 1/1 1/1 1/1 0/1 1/1 1/1 1/1 Total no. of G (-) 44/94 99/107 96/114 49/114 55/113 50/115 94/114 67/117 49/114 5/114 1/115 % of resistance 46.8 92.5 84.2 43.0 48.7 43.5 82.3 57.3 43.0 4.4 0.9 Resistance Pattern, GNB
- 16. Antibiotics Adults (≥ 20 years old) (n=140) Children (< 20 years old) (n=61) Penicillin 57 (40.7) 22 (36.1) 0.535 Cefotaxime 127 (90.7) 39 (65.0) < 0.001 Cefepime 120 (85.7) 39 (66.1) 0.002 Vancomycin 140 (100.0) 61 (100.0) NA Linezolid 140 (100.0) 60 (98.4) 0.303 Clindamycin 121 (86.4) 51 (83.6) 0.601 Erythromycin 78 (55.7) 21 (34.4) 0.006 Data from Catholic BMT Center [in press] Viridans Streptococci Bacteremia in NF
- 17. 초기 항균요법 (1) In contrast to western countries, Gram-negative bacteria are the prevailing etiological agents of infections in neutropenic fever patients in Asia. Because of the reported etiologic bacteria and their antimicrobial resistance rates causing neutropenic fever vary widely by times, area, even wards, every hospital should continue to monitor the changing patterns of etiology and adjustment of empirical antibiotics may be necessary. What is the major etiologic agents of neutropenic feverWhat is the major etiologic agents of neutropenic fever in Asia?in Asia?
- 18. J Antimicrob Chemother 2012;67:1311-20 Mortality: ESBL vs. Non-ESBL BSI
- 19. Ann Hematol 2013; [in press] ESBL vs. Non-ESBL BSI in NF No. (%) E. coli K. pneumoniae ESBL (n=15) Non-ESBL (n=72) ESBL (n=11) Non-ESBL (n=3) Age, median (range), yr 44 (15-64) 42 (17-74) 39 (16-59) 31 (23-42) Sex, M:F 9:6 39:33 6:5 3:0 Underlying disease AML ALL MM Others* 10 (66.7) 2 (13.3) 1 (6.7) 2 (13.3) 33 (45.8) 31 (43.1) 4 (5.6) 4 (5.6) 5 (45.5) 4 (36.4) 0 (0.0) 2 (18.1) 1 (33.3) 0 (0.0) 0 (0.0) 2 (66.6) Undergoing therapy Chemotherapy HSCT 10 (66.7) 5 (33.3) 59 (81.9) 13 (18.1) 8 (72.7) 3 (27.3) 3 (100.0) 0 (0.0) 1st set fever† 13 (86.7) 72 (100.0) 4 (36.3) 3 (100.0) Empirical therapy 3rd generation cephalosporin Cefepime Piperacillin-tazobactam Carbapenem Aminoglycoside combination 13 (87.0) 2 (13.0) 0 (0.0) 0 (0.0) 14 (93.3) 60 (83.0) 3 (4.0) 8 (11.1) 1 (1.4) 71 (98.6) 4 (36.0) 1 (9.0) 0 (0.0) 6 (54.5) 5 (45.5) 1 (33.3) 0 (0.0) 1 (33.3) 1 (33.3) 3 (100.0)
- 20. Ann Hematol 2013; [in press] Susceptibility
- 21. Characteristics Unadjusted OR (95% CI) p- value Adjusted OR (95% CI) p- value Disease status, non-remitted 3.569 (1.375-9.263) 0.009 - 0.110 History of ICU admission within prior 3 months 13.455 (1.429-126.686) 0.023 - 0.162 Hospital stay for >2 weeks within the preceding 3 months 7.874 (2.177-28.475) 0.002 5.887 (1.572-22.041) 0.008 Previous antibiotics use within the preceding 4 weeks Broad-spectrum cephalosporins 9.397 (2.584-34.179) 0.001 6.186 (1.616-23.683) 0.008 β-lactam/β-lactamase inhibitors 4.226 (1.040-17.173) 0.044 - 0.083 Aminoglycosides 6.088 (1.906-19.447) 0.002 - 0.565 Glycopeptides 8.690 (1.572-48.056) 0.013 - 0.436 Factors associated with ESBL BSI Ann Hematol 2013; [in press]
- 22. No. (%) E. coli K. pneumoniae ESBL (n=15) Non- ESBL (n=72) P ESBL (n=11) Non-ESBL (n=3) P Early response (72hr) CR PR Treatment failure 5 (33.3) 9 (60.0) 1 (6.7) 29 (40.3) 41 (56.9) 2 (2.8) NS 2 (18.2) 6 (54.5) 3 (27.3) 1 (33.3) 2 (66.7) 0 (0.0) NS Mortality Overall at 7 day at 30 day at EOT 0 (0.0) 1 (6.7) 5 1 (1.4) 3 (4.2) 30 (41.7) NS NS NS 0 (0.0) 2 (20.0) 9 (81.8) 0(0.0) 1 (33.3) 2 (66.7) NS NS NS Ann Hematol 2013; [in press] Factors associated with Mortality
- 23. Factors associated with Mortality Characteristics Unadjusted OR (95% CI) p-value Adjusted OR (95% CI) * p-value ESBL production 3.227 (0.745-13.982) 0.117 0.735 (0.231-2.338) 0.602 Inappropriate empirical antimicrobial therapy 4.286 (0.393-46.785) 0.233 1.401 (0.254-7.722) 0.699 Disease status, non-remitted 4.843 (1.131-20.735)* 0.034 1.990 (0.534-7.416) 0.305 Duration of neutropenia >3 weeks 7.731 (1.465-40.787) 0.016 1.757 (0.675-4.570) 0.248 Septic shock at presentation 43.500 (7.180-263.552) <0.001 2.946 (1.075-8.073) 0.036 Infecting organism, Klebsiella pneumoniae 8.300 (1.791-38.459) 0.007 3.593 (1.023-12.628) 0.046 Copathogen 7.731 (1.465-40.787) 0.016 1.335 (0.513-3.471) 0.554 Ann Hematol 2013; [in press]
- 24. EJC Suppl 2007;5:13-22 [ECIL-1] Role of Aminoglycoside in NF (1)
- 25. Role of Aminoglycoside in NF (2) Ann Hematol 2012;91:1161-74 [DGHO]
- 26. Role of Aminoglycoside in NF (3) While the addition of an aminoglycoside has not been shown to be of clinical advantage compared with beta-lactam monotherapy in systematic reviews, there are particular circumstances where the choice of aminoglycoside may be important. These include severe sepsis where there is a risk of resistance in Gram-negative bacilli and in Pseudomonas infection. Intern Med 2011;41:90-101 [Australian Guideline]
- 27. 초기 항균요법 (1) We still use the beta-lactam + aminoglycoside combination strategy for empirical therapy of NF. When ESBL is not proven, aminoglycoside is only used for 3-5 days. Adjustment for inadequate empirical therapy can lead to a reduction of mortality. For example, combination therapy with aminoglycoside… in high incidence of ESBL producingin high incidence of ESBL producing Enterobacteriaceae area…Enterobacteriaceae area…
- 28. PKs in Neutropenia Reduced serum, tissue, and body fluid concentrations of antibacterial agents have been reported in neutropenic patients and animal models, potentially reducing the bactericidal activities of these agents. PK changes in neutropenic patients are probably not only related to neutropenia per se, but also to the severity of sepsis, as has been in ICU patients. host defense mechanism… Lancet Infect Dis 2008;8:612-20
- 29. Lancet Infect Dis 2008;8:612-20 PK of Glycopeptides in Neutropenia
- 30. What can we learn from studies comparing Linezolid with Vancomycin in neutropenic patients when vancomycin doses are not optimized? Clin Infect Dis 2006;42:1813-4 1. PK of vancomycin therapy in neutropenic patients is different. ; 3-fold increases of initial Vd, shorted half-life (vs. healthy volunteer) 2. Achievement of trough serum conc. ≥15 mg/L? 3. T>MIC 100% 4. 1 g iv q12hrs fixed dose 30 mg/kg/day
- 31. Vancomycin TDM Consensus Am J Health Syst Pharm 2009;66:82-98
- 32. Antimicrob Agents Chemother 2001;45:2460-7 Continuous vs. Intermittent Infusion of Vancomycin in Severe Staphylococcal InfectionFrance, Prospective study, CIV (plateau 20-25 mg/L), IIV (trough 15-20 mg/L) N= 119, Hospital acquired infection, bacteremia 35%, pneumonia 45%
- 33. Empirical Teicoplanin in Neutropenic Fever in Korea: Comments TPV 400 mg qd and then 200 mg qd ; is that enough? 1. Only one strains of S. aureus, 2. CNS can be affected by catheter removal 3. Four out of 6 strains of E. faecium were vancomycin resistant. 4. Viridans streptococci would be susceptible with cefepime. Infect Chemother 2004;36:83-91
- 34. J Antimicrob Chemother 2003;51:971-5 Loading Dose of Teicoplanin
- 35. Teicoplanin Dose in Acute Leukemia and Febrile Neutropenia Clin Pharmacokinet 2004;43:405-15
- 36. Yonsei Med J 2011;52:616-23
- 37. 초기 항균요법 (1) PK of glycopeptides in neutropenic patients is different with that of normal volunteers. We need their PK data!!! may need higher doses than usual Vancomycin trough concentrations 15-20 mg/L or AUC/MIC >400 would be required in neutropenic fever as well as in severe staphylococcal infection. Teicoplanin PK/PD magnitude for neutropenic fever is not established yet (trough >10 or 20 mg/L, AUC/MIC >345??). However, TDM would be needed for monitoring TAR. Teicoplanin dose would be needed more than we usually prescribe. When using glycopeptide to NF patients, Consider…When using glycopeptide to NF patients, Consider…
- 38. Summary Etiology of NF is different according to the area, time, even the wards in the same hospital. We need to continue monitoring the changing patterns. ESBL producing organisms are common. High index of suspicion (prior use of beta-lactams, Hx of long hospital stay…) is important. For empirical Tx against ESBL organisms, consider the susceptibility patterns and adjust for inadequate antibiotics… PK of glycopeptides in neutropenic patients is different with that of normal volunteers. We need their PK data!!! Population PK
- 39. Thank You for Your Attention


![Clin Infect Dis 2003;36:1103-10
Epidemiology, US [SCOPE] Project](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-4-320.jpg)











![Antibiotics Adults
(≥ 20 years old)
(n=140)
Children
(< 20 years old)
(n=61)
Penicillin 57 (40.7) 22 (36.1) 0.535
Cefotaxime 127 (90.7) 39 (65.0) < 0.001
Cefepime 120 (85.7) 39 (66.1) 0.002
Vancomycin 140 (100.0) 61 (100.0) NA
Linezolid 140 (100.0) 60 (98.4) 0.303
Clindamycin 121 (86.4) 51 (83.6) 0.601
Erythromycin 78 (55.7) 21 (34.4) 0.006
Data from Catholic BMT Center [in press]
Viridans Streptococci Bacteremia in
NF](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-16-320.jpg)


![Ann Hematol 2013; [in press]
ESBL vs. Non-ESBL BSI in NF
No. (%)
E. coli K. pneumoniae
ESBL
(n=15)
Non-ESBL
(n=72)
ESBL
(n=11)
Non-ESBL
(n=3)
Age, median (range), yr 44 (15-64) 42 (17-74) 39 (16-59) 31 (23-42)
Sex, M:F 9:6 39:33 6:5 3:0
Underlying disease
AML
ALL
MM
Others*
10 (66.7)
2 (13.3)
1 (6.7)
2 (13.3)
33 (45.8)
31 (43.1)
4 (5.6)
4 (5.6)
5 (45.5)
4 (36.4)
0 (0.0)
2 (18.1)
1 (33.3)
0 (0.0)
0 (0.0)
2 (66.6)
Undergoing therapy
Chemotherapy
HSCT
10 (66.7)
5 (33.3)
59 (81.9)
13 (18.1)
8 (72.7)
3 (27.3)
3 (100.0)
0 (0.0)
1st
set fever†
13 (86.7) 72 (100.0) 4 (36.3) 3 (100.0)
Empirical therapy
3rd
generation cephalosporin
Cefepime
Piperacillin-tazobactam
Carbapenem
Aminoglycoside combination
13 (87.0)
2 (13.0)
0 (0.0)
0 (0.0)
14 (93.3)
60 (83.0)
3 (4.0)
8 (11.1)
1 (1.4)
71 (98.6)
4 (36.0)
1 (9.0)
0 (0.0)
6 (54.5)
5 (45.5)
1 (33.3)
0 (0.0)
1 (33.3)
1 (33.3)
3
(100.0)](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-19-320.jpg)
![Ann Hematol 2013; [in press]
Susceptibility](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-20-320.jpg)
![Characteristics
Unadjusted OR (95% CI) p-
value
Adjusted OR (95%
CI)
p-
value
Disease status, non-remitted
3.569 (1.375-9.263) 0.009
- 0.110
History of ICU admission within prior 3 months 13.455 (1.429-126.686) 0.023
- 0.162
Hospital stay for >2 weeks within the preceding 3 months 7.874 (2.177-28.475) 0.002
5.887 (1.572-22.041) 0.008
Previous antibiotics use within the preceding 4 weeks
Broad-spectrum cephalosporins
9.397 (2.584-34.179) 0.001
6.186 (1.616-23.683) 0.008
β-lactam/β-lactamase inhibitors
4.226 (1.040-17.173) 0.044
- 0.083
Aminoglycosides
6.088 (1.906-19.447) 0.002
- 0.565
Glycopeptides
8.690 (1.572-48.056) 0.013
- 0.436
Factors associated with ESBL BSI
Ann Hematol 2013; [in press]](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-21-320.jpg)
![No. (%)
E. coli K. pneumoniae
ESBL
(n=15)
Non-
ESBL
(n=72)
P
ESBL
(n=11)
Non-ESBL
(n=3)
P
Early response (72hr)
CR
PR
Treatment failure
5
(33.3)
9
(60.0)
1 (6.7)
29 (40.3)
41 (56.9)
2 (2.8)
NS
2 (18.2)
6 (54.5)
3 (27.3)
1 (33.3)
2 (66.7)
0 (0.0)
NS
Mortality
Overall
at 7 day
at 30 day
at EOT
0 (0.0)
1 (6.7)
5
1 (1.4)
3 (4.2)
30 (41.7)
NS
NS
NS
0 (0.0)
2 (20.0)
9 (81.8)
0(0.0)
1 (33.3)
2 (66.7)
NS
NS
NS
Ann Hematol 2013; [in press]
Factors associated with Mortality](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-22-320.jpg)
![Factors associated with Mortality
Characteristics Unadjusted OR (95% CI) p-value Adjusted OR (95% CI) *
p-value
ESBL production 3.227 (0.745-13.982) 0.117 0.735 (0.231-2.338) 0.602
Inappropriate empirical antimicrobial therapy 4.286 (0.393-46.785) 0.233 1.401 (0.254-7.722) 0.699
Disease status, non-remitted 4.843 (1.131-20.735)*
0.034 1.990 (0.534-7.416) 0.305
Duration of neutropenia >3 weeks 7.731 (1.465-40.787) 0.016 1.757 (0.675-4.570) 0.248
Septic shock at presentation 43.500 (7.180-263.552) <0.001 2.946 (1.075-8.073) 0.036
Infecting organism, Klebsiella pneumoniae 8.300 (1.791-38.459) 0.007 3.593 (1.023-12.628) 0.046
Copathogen 7.731 (1.465-40.787) 0.016 1.335 (0.513-3.471) 0.554
Ann Hematol 2013; [in press]](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-23-320.jpg)
![EJC Suppl 2007;5:13-22 [ECIL-1]
Role of Aminoglycoside in NF (1)](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-24-320.jpg)
![Role of Aminoglycoside in NF (2)
Ann Hematol 2012;91:1161-74
[DGHO]](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-25-320.jpg)
![Role of Aminoglycoside in NF (3)
While the addition of an aminoglycoside has not been shown to
be of clinical advantage compared with beta-lactam
monotherapy in systematic reviews, there are particular
circumstances where the choice of aminoglycoside may be
important. These include severe sepsis where there is a risk
of resistance in Gram-negative bacilli and in
Pseudomonas infection.
Intern Med 2011;41:90-101 [Australian Guideline]](https://image.slidesharecdn.com/neutropenicfever-dgl-130823182952-phpapp01/85/Neutropenic-fever-Challenges-and-Treatment-26-320.jpg)












