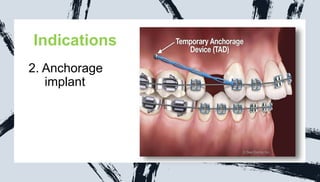
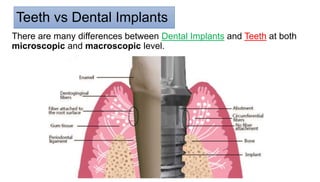
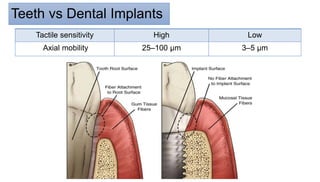
The document discusses peri-implant pathology and its components, including indications, contraindications, and classifications of dental implants, as well as the conditions of peri-implant mucosa and diseases like peri-implant mucositis and peri-implantitis. It outlines the differences between natural teeth and dental implants, the risk factors associated with implant diseases, and the management strategies for maintaining healthy peri-implant tissues. Ultimately, the document emphasizes the importance of proper oral hygiene and treatment options for preventing and managing inflammatory conditions surrounding dental implants.