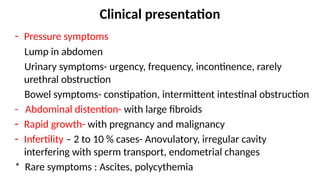
Uterine fibroids, also known as leiomyomas, are the most common benign tumors in the uterus, affecting 20-40% of reproductive-age women. Their etiology involves genetic and hormonal factors, and they can present with a range of symptoms, including abnormal uterine bleeding, pelvic pain, and pressure symptoms. Management options vary from watchful waiting for asymptomatic cases to various medical and surgical interventions depending on symptoms and patient desire for fertility.












































![REFERENCES
• Shaw’s Textbook of Gynecology Chapter 29 Benign Disease of the
Uterus
• Barjon K, Mikhail LN. Uterine Leiomyomata. [Updated 2023 Aug
7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls
• Buttram VC Jr, Reiter RC. Uterine leiomyomata: etiology,
symptomatology, and management.
• Dewhurst's Textbook of Obstetrics & Gynaecology, Chapter 59
Benign Disease of the Uterus](https://image.slidesharecdn.com/uterinefibroidpresentation-241208114006-8a0de2fe/85/Uterine-Fibroid-Presentation-for-ONGpptx-47-320.jpg)
